Table of Contents
People have only two dentition: milk and permanent teeth. After the permanent teeth replace milk, in case of loss of permanent teeth there is no longer a third generation of natural teeth which can replace them. Tooth loss, regardless of the cause of loss, brings the question of its replacement: ”Should I replace the lost tooth? If it needs to be replaced, what is the best thing to do?”
The reasons for tooth loss are numerous, from the extraction due to pathological changes in the tooth and associated tissues (deep caries, periapical and periodontal disease, etc.) to traumatic tooth injury.
 In any case, after a tooth is lost and removed from the mouth, an empty space remains in his place. If the extracted tooth was at the end of a complete teeth arch (i.e. the third molar), its loss has no major impact on functional ability and aesthetic value of such system, as it would be the case if that was a tooth located between two other teeth in the same jaw. With the appearance of an empty space between two adjacent teeth, due to loss of support that was provided by extracted tooth, these teeth begin to change their position and fill the void by leaning and rotating. This reduces chewing ability of dental system, and in addition, in the case of the tooth that was located in the visible part of the teeth arch, leads to poor aesthetic appearance of the patient.
In any case, after a tooth is lost and removed from the mouth, an empty space remains in his place. If the extracted tooth was at the end of a complete teeth arch (i.e. the third molar), its loss has no major impact on functional ability and aesthetic value of such system, as it would be the case if that was a tooth located between two other teeth in the same jaw. With the appearance of an empty space between two adjacent teeth, due to loss of support that was provided by extracted tooth, these teeth begin to change their position and fill the void by leaning and rotating. This reduces chewing ability of dental system, and in addition, in the case of the tooth that was located in the visible part of the teeth arch, leads to poor aesthetic appearance of the patient.
It is best to compensate tooth lost in some way as soon as possible. If the patient waits with the replacement, due to changes in the position of adjacent teeth, surgery may become much more complex and expensive than the replacement accessed immediately after tooth loss.
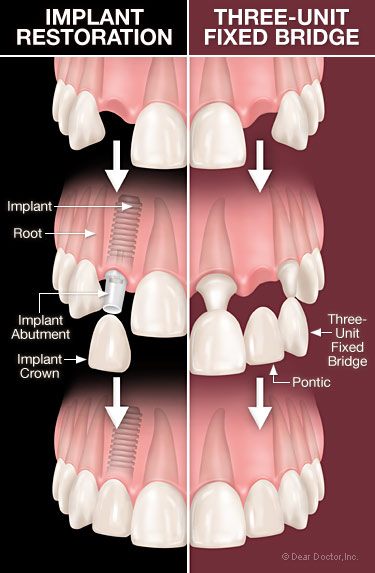
There are two possibilities for the replacement of lost or missing tooth. One is the creation of the dental bridge. Another option is to install it at the place of the previously lost tooth.
The dilemma whether a tooth with a poor prognosis should treat conservatively and keep it in the mouth as long as possible to avoid dentures or remove it, today is a lot easier to resolve because the tooth can easily be replaced.
What is it?
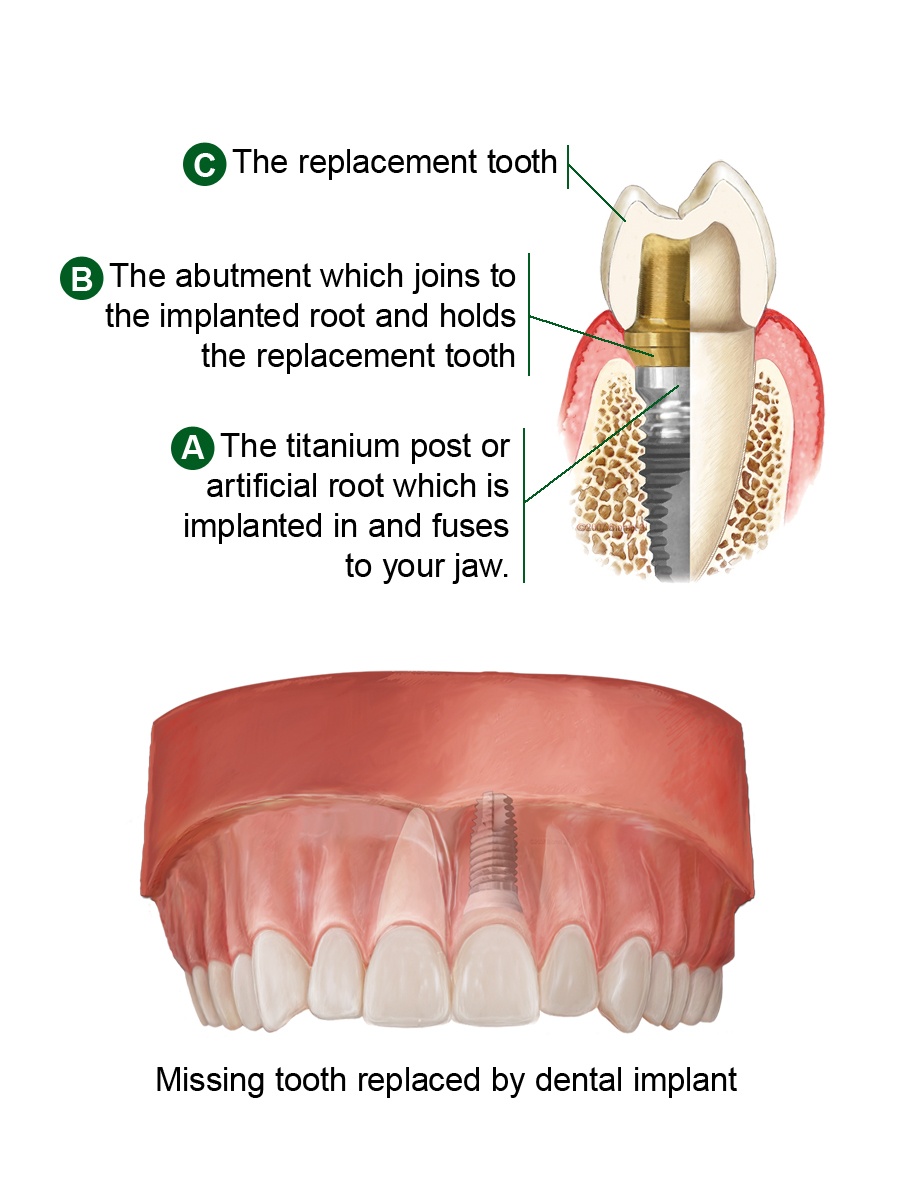
It is defined as an artificial tooth root used in dentistry as a replacement of one or more teeth. In other words, a dental implant eliminates the need for grinding of adjacent teeth (which are often healthy and intact) because it can serve as a carrier of crowns, bridges or removable dentures.
 Nowadays they are placed into the jawbone and are built of titanium screws whose shape more or less mimics the tooth root. The surface of the titanium screws can be rough or smooth.
Nowadays they are placed into the jawbone and are built of titanium screws whose shape more or less mimics the tooth root. The surface of the titanium screws can be rough or smooth.
They are based on the idea of osseointegration – the tendency to create a direct connection between the bone and them, without the inserted layers of soft tissue.
A successful osseointegration occurs when there is clinically asymptomatic rigid bond between alloplastic material from which it was made and the bone itself.
In the past, they were incorporated by specialists in oral surgery in cooperation with specialists in prosthodontics, but today they are so widespread in the world so dentists without formal education as specialists install them as well. To this has probably contributed not only their continuous improvement and of related technologies, which resulted in an increased percentage of their efficacy, but also higher awareness among patients about the importance of preserving their own teeth and oral health. However, in any case, but especially in the case of extensive rehabilitation, the cooperation between oral surgeon and prosthodontist is preferred. Oral surgeon assesses the quality of the bone, its height, width and relationship to surrounding anatomic structures, while the dentist – a prosthetic specialist assesses whether the prosthetic rehabilitation by the installation of dental implants is appropriate or better functional and aesthetic results can be achieved with conventional prosthetic replacement (dental bridge).
For whom are they intended?
In order the replacement of the lost teeth with dental implants was functionally and aesthetically successful and long-term, it is necessary to set up a good indication for their installation.
 In general, the indications for the installation of dental implants are toothless lower and/or upper jaw, partial edentulism or lack of a single tooth.
In general, the indications for the installation of dental implants are toothless lower and/or upper jaw, partial edentulism or lack of a single tooth.
They can also be installed if the patient has dentures with poor retention and stability which makes him dissatisfied. In addition, if the arrangement of the remaining teeth in the jaw is such that it does not guarantee a functional and aesthetic look made by conventional methods (dental bridge), it is desirable to install an implant. Sometimes patients also insist on the so-called “considerate treatment” and do not want their teeth to be shaped for dental bridge. In such situations, it is the only choice.
If indications are met, and there are no contraindications, they can be installed for all adults. The completion of the growth of the upper or lower jaw is considered a minimum age for their installation. This means in principle that implants in people younger than 16 are not recommended.
When are they not recommended?
Although with the help of dental implants dentists often can create a prosthetic that will have greater functional and aesthetic value than conventional dental bridge, there are times when they are not recommended. In addition to the already mentioned lower age limit, contraindications for their use may include: local, general medical, temporary and contraindications caused by mental states.
Local contraindications are unfavorable anatomic relationships of the jaw, inadequate occlusal relationships and functional disorders, pathological changes in the jaw bone and the oral mucosa, poor oral health, poor oral hygiene, and dry mouth.
General medical contraindications for placement of dental implants are: poor general health, collagenosis, rheumatoid arthritis, Sjögren’s syndrome, diseases of the skeletal system (e.g. osteomalacia, osteoporosis) and metabolic diseases. Juvenile diabetes is considered an absolute contraindication, while the maturity-onset diabetes is considered a relative contraindication for implant placement. Because of the bleeding that occurs during implant installation, hematological diseases, hemorrhagic diathesis and diseases of erythrocytes and leukocytes are considered absolute contraindications for dental implants.
In patients with heart disease and circulatory system diseases, prior to implant placement, consultation with a physician who is treating the primary disease is required. Patients with artificial heart valves, and a history of endocarditis belong to the group of high risk patients for implant placement.
As temporary contraindications are considered: taking certain medications (corticosteroids, immunosuppressants), smoking, pregnancy, acute inflammatory diseases and infections.
The group of contraindications caused by mental states include: neurosis and psychosis, consummation of alcohol and drugs, lack of cooperation of the patient and emotional instability.
 How are they installed?
How are they installed?
Installation procedure is carried out according to a specific protocol recommended by the manufacturer of dental implants. The dental implant installation procedure is preceded by the preparation of the patient which includes: taking a detailed medical and dental history, clinical examination and assessment of the anatomical structures of the mouth and jaw, a detailed X-ray image analysis, making models of jaws and registration of jaw relationship.
Patient’s preparation also includes detailed introduction to the length of therapy procedure, its results, prognosis and possible complications, both in operating and postoperative period, after which the patient needs to sign a written consent to dental treatment.
The process of installation is a surgical procedure under sterile conditions with the use of specific equipment and instruments. The person who carries out the procedure must be well trained to implement and to operate. To ensure painless operation, before surgery the patient is given local anesthesia. When the anesthesia takes effect, oral surgeon carefully removes the oral mucosa and reveals the bone which is below. Into the bone an opening of certain diameter is cut into which the implant is inserted. After that a blanking plug is placed on the implant and then removed oral mucosa is sewed so that the implant can not be seen. Depending on the number of implants to be installed, the operation can vary from 30 to 60 minutes.
Upon completion of the insertion of dental implant in bone, it takes several months for osseointegration process to appear and form a solid connection between the bone and the implant. Studies have shown that in lower jaw it takes an average three months to lead to osseointegration, while in the upper jaw it needs about six months. During this period, for aesthetic and functional reasons, a temporary prosthetic replacement is provided to the patient.
When, after this period of healing, surgeon finds that there has been osseointegration, a second operation needs to be done. Each movement of the implant, even the smallest, indicates that osseointegration process failed. During the second surgery oral mucosa above the implant is carefully opened, the blanking plug is removed and abutment is installed (the basis on which the crowns, bridges or dentures are placed).
Besides the already described procedure, today there are systems in which it is possible to place the crown on it immediately after its posted into the bone. However, this is possible only in strictly defined cases.
Are complications possible?
As with all surgeries, there is always the possibility of complications. By installing them according to the rules and respect the recommendations of manufacturers , the possibility of complications is reduced to a minimum. According to some studies, the success rate is higher than 97%.
Complications related to procedure are divided into early and late complications.
Early complications arise before the osseointegration process appears and are related to: implant itself and surgical technique (e.g. nerve damage or opening of the maxillary sinus), the patient’s health status and condition of the jaw bone.
Late complications occur after the end of osseointegration process and after placing a prosthetic superstructure over it (abutment and crown). The most common are inflammation (periimplantitis – inflammation in jaw bone that surrounds dental implant), pain sensations and its overload due to the poor volume and quality of existing bone.
The destructive inflammatory process that affects the soft and hard tissues in contact with it is called periimplantitis. Depending on the research criteria, frequency of periimplantitis is 11-47 percent.
Sometimes it happens that the patient’s organism sees it as a foreign body and seeks to reject it. In these situations osseointegration process is deficient, and it is not a good solution for compensation of missing teeth. Unfortunately, this complication except theoretically is not possible to predict.

In the period after implant placement, and before making a prosthetic superstructure (dental crown), the pressure on the implant must be disabled to avoid its overload in the phase of osseointegration. Implant overload can occur even when the prosthetic rehabilitation (dental bridge or denture) is badly planned, so one implant becomes a carrier that replaces more teeth. Overloading the implant significantly reduces its life.
Although they are made of metal (today the most commonly titanium), in some situations they can still unpredictably bend and break. In such situations, the implant should be removed and replaced, and the cause of breaking should be determined.
Gums that surround natural teeth may, due to various reasons, become inflamed. If the inflammation affects only the gums we are talking about gingivitis. But if deeper layers of the support system of teeth are affected, including the bone, then we are talking about periodontitis. The loss of bone around the roots of adjacent teeth leads to loosening these teeth and, depending on the extent of the bone loss, to their falling out. Similarly it can happen with dental implants. If the bone loss is so great that it is not standing firmly in bone then implant therapy has failed. The loss of bone that surrounds the dental implant can be monitored by the X-rays.
In patients who, for the treatment of metabolic and pathological changes of the skeletal system, are taking bisphosphonates, it is possible that process of implant osseointegration becomes slow or incomplete. Therefore, any patient taking bisphosphonates should be individually assessed and treated in cooperation with the doctor who is treating the primary disease.
How to maintain dental implants?
Installation requires not only good previous diagnostic treatment, but also a good estimate of the patient. In order for a dental implant to stay as long as possible in the mouth and perform its intended role, it is desirable that the patient be motivated for its maintenance.
The patient is expected to cooperate with the dentist, to regularly come for check-ups and impeccably maintain oral hygiene. The dentist will, depending on the clinical situation and the characteristics of a prosthetic device, each patient with implants refer to the specifics of hygiene in the area around the dental implant.
How much do dental implants cost?
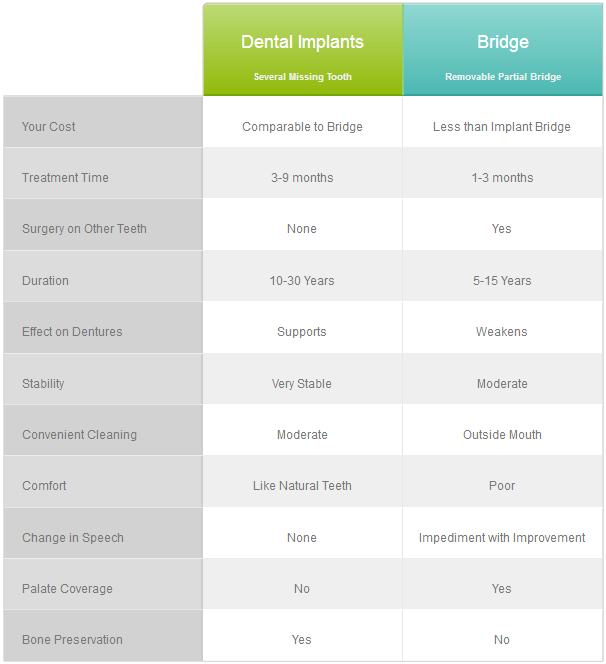
They have many advantages over conventional fixed or mobile prosthetic restorations. However, one of the reasons why they will not soon completely displace conventional prosthetic solutions it is their price. Their cost is still higher than the price of dental bridge. In the long term, this higher price is worth it, both for functionality, aesthetic value, and because of their long life cycle.
What is the lifetime of dental implants?
Likewise natural teeth, they can not last forever. The durability of the implants depends on several factors which are divided into two groups. First group includes factors related to the applied surgical technique, prosthetic work, the implant material and the surface characteristics and shape of the implant. Second group includes factors related to the patient from the general medical health status to everyday life and oral hygiene habits. If their installation was carried out according to the rules and with respect to the recommendations of implant manufacturers, with proper oral hygiene and maintenance and no significant changes of general and oral health of the patient, it is considered that the implant can function in the oral cavity between 5 and 20 years. Wheather you have dental implant or a bridge your oral health will be much better with proper daily routine in which you should definetly consider including a Waterpik water flosser.
Conclusion
They are excellent, if not all-powerful, solution that goes beyond the numerous disadvantages of conventional prosthetic appliances (dental bridges and dentures). Their advantages are primarily in better aesthetics, functionality, reliability and the fact that no unnecessary shaping of healthy teeth is needed. Although they are much better solution (not necessarily financially most acceptable) than conventional prosthetic substitutes, during implant placement it is important to meet all necessary indications. Any potential contraindication should be carefully analyzed and, in accordance with, finally decide whether the implant is the best solution for the individual patient.