Diabetes (lat. Diabetes mellitus) is a chronic disease characterized by elevated blood glucose level and metabolic disorders of carbohydrates, fats and proteins. Diabetes is caused by two reasons: when the pancreas stops completely or partially to produce hormone insulin (Type 1 diabetes) or when the insulin is not effective in the body (Type 2 diabetes).
Type 1 diabetes (formerly called insulin dependent type) occurs in 10% of patients, most often in children and adolescents. The etiology of this disease is still unclear. It is believed that this type of diabetes occurs as a result of an autoimmune destruction of insulin-producing beta cells in the pancreas (pancreatic islets, also called islets of Langerhans – tiny clusters of cells scattered throughout the pancreas). The disease has a sudden start with the appearance of symptoms such as frequent urination, excessive thirst, constant hunger, pronounced fatigue and lack of energy.
 Type 2 diabetes (formerly called non-insulin dependent type) occurs in 90% of patients, mainly adults over forty years of age. The disease occurs when the pancreas is not anymore able to produce sufficient amounts of hormone insulin to meet the needs of the organism or when the target cells become resistant to insulin (target cells – cells which contain insulin receptors such as liver, muscle and fat cells). Symptoms of the disease develop gradually, are milder in intensity and in approximately 50% of cases are not present until the development of chronic complications. The most important risk factor for the development of type 2 diabetes is being overweight. At the time of diagnosis 60 to 80% of patients are overweight.
Type 2 diabetes (formerly called non-insulin dependent type) occurs in 90% of patients, mainly adults over forty years of age. The disease occurs when the pancreas is not anymore able to produce sufficient amounts of hormone insulin to meet the needs of the organism or when the target cells become resistant to insulin (target cells – cells which contain insulin receptors such as liver, muscle and fat cells). Symptoms of the disease develop gradually, are milder in intensity and in approximately 50% of cases are not present until the development of chronic complications. The most important risk factor for the development of type 2 diabetes is being overweight. At the time of diagnosis 60 to 80% of patients are overweight.
Without timely diagnosis, patients with diabetes have a distinct risk of dangerous complications. Complications include pathological changes in the kidneys (diabetic nephropathy), retina of the eye (diabetic retinopathy), accelerated occurrence of atherosclerotic changes which increase the risk for appearance of heart attack, stroke or gangrene. A patient with diabetes has twenty-five times greater risk of kidney failure and twenty times higher risk of blindness compared with a healthy person. The risk of developing heart attacks and strokes in these patients are increased two to five times compared to the healthy population.
Oral manifestations of diabetes
Besides previous mentioned complications, diabetes can also manifest with pathological changes and symptoms in the oral cavity. Moreover, the dentist may be the first health professional to suspect on presence of diabetes and refer patient for further examinations and treatment. Oral manifestations of diabetes are gingivitis and periodontitis, dry mouth, increased susceptibility to infections especially fungal, increased susceptibility to caries, burning sensation of oral mucosa and difficult wound healing.
Gingivitis and periodontitis are the most common oral complications of diabetes. Although both gingivitis and periodontal disease primarily are caused by bacteria from dental plaque, patients with diabetes have a three times greater risk of developing gingivitis and periodontitis compared with healthy population. There are several reasons for this. In patients with poorly controlled diabetes the number of destructive bacteria (spirochetes and movable rods) is increased than in patients with well-controlled diabetes and non-diabetic individuals.
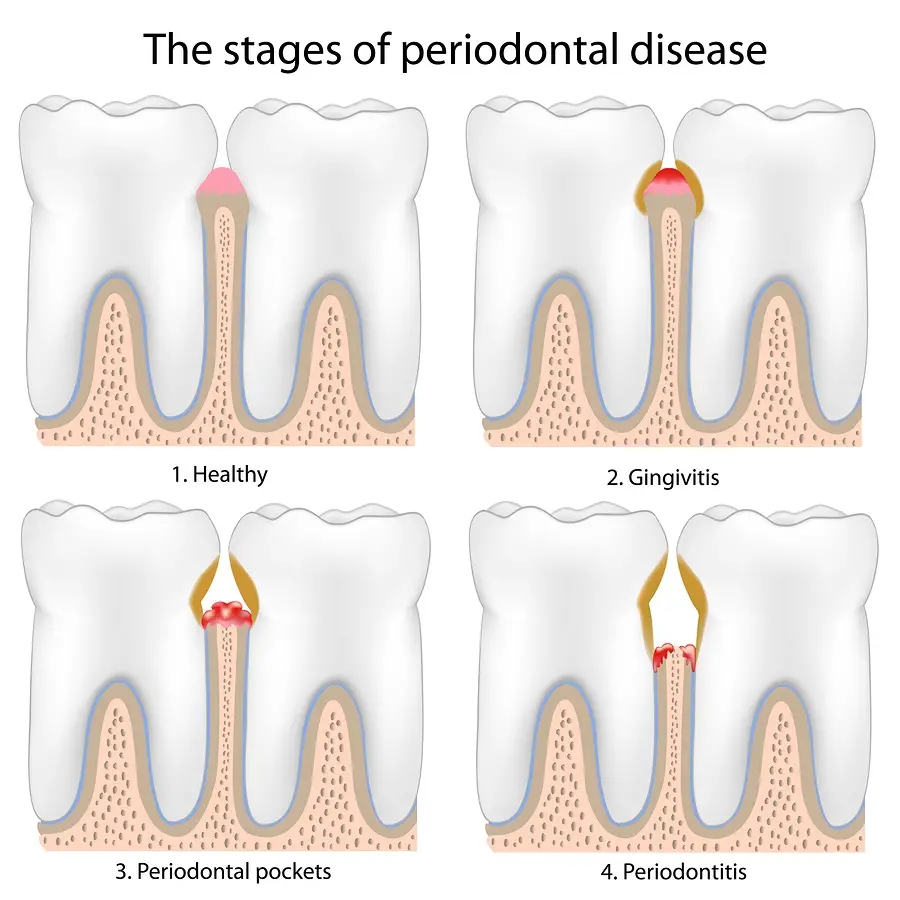 There are also changes in the inflammatory response of the body – polymorphonuclear leukocytes (cells that are responsible for defense of organism) have reduced ability to migrate and they secrete more inflammatory mediators and proteolytic enzymes. All of this leads to more destruction of dental tissue than is the case in the normal healthy population.
There are also changes in the inflammatory response of the body – polymorphonuclear leukocytes (cells that are responsible for defense of organism) have reduced ability to migrate and they secrete more inflammatory mediators and proteolytic enzymes. All of this leads to more destruction of dental tissue than is the case in the normal healthy population.
The healing of tissue is hampered, synthesis of collagen in connective tissue cells is decreased and newly synthesized collagen is a biologically less valuable and is subject to faster degradation. Pathological changes in the small blood vessels also contribute to slower healing, due to which there is a lower supply of oxygen to tissues and slower removal of decay material from tissue caused by inflammation. Because of this, gingivitis and periodontal disease in patients with diabetes are more severe, accompanied by a greater degree of inflammation and tissue destruction and less responsive to treatment.
It is significant that if the diabetes is well-controlled, risk of developing the gingivitis and periodontal disease becomes a similar to risk in healthy population. In well-controlled diabetes, the response to periodontal therapy is also improved.
 The relation between periodontal disease and diabetes is not a one-way relationship. Periodontal disease as well has a negative impact on the control of blood sugar levels and increases the risk of other complications of diabetes. In the study of Scandinavian authors, patients with diabetes and severe periodontitis have had almost four times more complications (higher cardiovascular, cerebrovascular or peripheral vascular events) compared to diabetic patients with mild periodontitis. Also, if the treatment of periodontitis is well-established, there is also better control of blood sugar levels.
The relation between periodontal disease and diabetes is not a one-way relationship. Periodontal disease as well has a negative impact on the control of blood sugar levels and increases the risk of other complications of diabetes. In the study of Scandinavian authors, patients with diabetes and severe periodontitis have had almost four times more complications (higher cardiovascular, cerebrovascular or peripheral vascular events) compared to diabetic patients with mild periodontitis. Also, if the treatment of periodontitis is well-established, there is also better control of blood sugar levels.
Dry mouth is a common complaint of patients with diabetes. It occurs due to dehydration of the body caused by frequent urination (polyuria). The loss of saliva causes many unpleasant symptoms – mucosa becomes sick, vulnerable and susceptible to injury. In some patients there is also difficulty in wearing dentures. This may ultimately result in disordered eating and avoiding meals, which will have a negative impact on blood sugar regulation. Lack of saliva leads to increased accumulation of dental plaque that contributes to periodontal disease and increases the risk of cavities. The saliva of patients with uncontrolled diabetes is richer with glucose, which favors the development of microorganisms and the formation of oral infections.
 Oral candidiasis is the most common infection of the oral cavity in uncontrolled diabetes. The cause of this infection is the fungus Candida albicans which is part of the normal microbial flora of the oral cavity. Only in case of disruption of local or systemic immunity of the body, this opportunistic fungus reproduces uncontrollably and causes a infection. Candidiasis may manifest as several clinical forms: as pseudomembranous candidiasis, atrophic candidiasis, hyperplastic candidiasis, medial rhomboid glossitis or angular cheilitis. Other factors also contribute to the development of infection such as lack of saliva (dry mouth), disturbed immune response and a higher level of glucose in the saliva. Besides oral candidiasis, in patients with uncontrolled diabetes are described cases (although rare) of deep and severe fungal infections accompanied by the formation of extensive ulcerations and widespread destruction of tissue.
Oral candidiasis is the most common infection of the oral cavity in uncontrolled diabetes. The cause of this infection is the fungus Candida albicans which is part of the normal microbial flora of the oral cavity. Only in case of disruption of local or systemic immunity of the body, this opportunistic fungus reproduces uncontrollably and causes a infection. Candidiasis may manifest as several clinical forms: as pseudomembranous candidiasis, atrophic candidiasis, hyperplastic candidiasis, medial rhomboid glossitis or angular cheilitis. Other factors also contribute to the development of infection such as lack of saliva (dry mouth), disturbed immune response and a higher level of glucose in the saliva. Besides oral candidiasis, in patients with uncontrolled diabetes are described cases (although rare) of deep and severe fungal infections accompanied by the formation of extensive ulcerations and widespread destruction of tissue.
Burning sensation of the oral mucosa (burning mouth syndrome), in the absence of any pathological changes, also often occurs in patients with diabetes. Burning can be the result of reduced amount of saliva and consequently higher sensitivity of mucous membranes. Less frequently, burning symptom can be a consequence of diabetic neuropathy, a complication of diabetes that affects the sensory and motor nerves. The literature describes several instances in which the burning sensation in the tongue was the first manifestation of diabetes.
Dental treatment of patients with diabetes
In the dental treatment of patients with diabetes, the most important is to have good communication with the patient. Before treatment, the dentist needs to know which therapy is the patient taking, is the disease under control and whether there are complications on vital organs. If the disease is under control and the blood glucose level is within acceptable limits and the patient has no complications on vital organs, all dental procedures can be carried out normally.
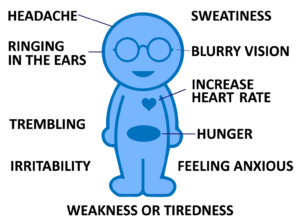 For patients who are treated with insulin it is recommended to visit a dentist in the morning. It is necessary to take the usual dose of insulin and not to skip breakfast. Skipping meals increases the risk of hypoglycemia during dental procedure. If during the procedure the patient feels symptoms of hypoglycemia (weakness, dizziness, tingling in the body, sweating, rapid heartbeat, red dry skin, rapid breathing, dehydration, acetone breath) or dentist notices that the patient is disoriented, dizzy or looks like he was drunk, treatment should be discontinued and the patient immediately given sweetened drink, candy bar or another “quick bite” sugar.
For patients who are treated with insulin it is recommended to visit a dentist in the morning. It is necessary to take the usual dose of insulin and not to skip breakfast. Skipping meals increases the risk of hypoglycemia during dental procedure. If during the procedure the patient feels symptoms of hypoglycemia (weakness, dizziness, tingling in the body, sweating, rapid heartbeat, red dry skin, rapid breathing, dehydration, acetone breath) or dentist notices that the patient is disoriented, dizzy or looks like he was drunk, treatment should be discontinued and the patient immediately given sweetened drink, candy bar or another “quick bite” sugar.
Hypoglycemia is the most dangerous complication that can occur during dental treatment of patients with diabetes and needs to be recognized and treated because it can be fatal!
 Although symptoms of hypoglycemia may resemble to symptoms of vasovagal reaction (sudden pressure drop caused by stress due to dental procedure), the difference is that when it comes to hypoglycemia there is no improvement after patient is lowered to a horizontal position.
Although symptoms of hypoglycemia may resemble to symptoms of vasovagal reaction (sudden pressure drop caused by stress due to dental procedure), the difference is that when it comes to hypoglycemia there is no improvement after patient is lowered to a horizontal position.
In the case when more extensive dental surgery is needed and when it is expected that food intake will be difficult in the next few days, it is necessary to consult a physician in order to adjust the dose of insulin and diet. Meals should not be skipped on patient’s own initiative, the food should be soft and mushy, but with the recommended composition and energy value. In a well-controlled diabetics, routine administration of antibiotics after the surgical procedure is not recommended. Antibiotics should be administered only in the case of the development of acute infection.
The decision of administering antibiotics is made for each patient individually based on the clinical situation and the general condition of the patient.
In case when the disease is not well controlled and when the blood glucose level is below 3.8 mmol/L or above 11.1 mmol/L, it is recommended to perform only emergency dental procedures. Other procedures should be postponed until blood sugar levels is under control.
If the patient has a complication of the disease present (such as nephropathy, atherosclerotic changes, heart attack or stroke in the past six months), also only emergency procedures and consultation with a physician are recommended. The physician will assess the general health of the patient and the dentist will, accordingly, adjust further dental treatment. In patients with severe renal impairment nephrotoxic drugs (acyclovir, non-steroidal anti-inflammatory drugs, acetaminophen in high doses) should be avoided and blood pressure should be controlled during dental treatment. Blood pressure control during dental treatment is also recommended in patients with cardiovascular complications.
In patients with poorly controlled diabetes, wound healing is difficult and risk of infection is increased.
 Regular dental checkups and cleanings of soft and hard teeth deposits are recommended every three months, and more often if necessary. It is very important to warn patients of the importance of oral hygiene. All acute infections should be aggressively treated. For the prevention of tooth decay, it is recommended to use preparations of fluoride, If necessary, preparations of artificial saliva can be administered.
Regular dental checkups and cleanings of soft and hard teeth deposits are recommended every three months, and more often if necessary. It is very important to warn patients of the importance of oral hygiene. All acute infections should be aggressively treated. For the prevention of tooth decay, it is recommended to use preparations of fluoride, If necessary, preparations of artificial saliva can be administered.
A dentist has an important role in the detection of undiagnosed cases of diabetes!
 All patients with extensive periodontal disease which responds poorly to therapy, patients with frequent episodes of candidiasis and patients with severe dryness of the mouth (especially if they complain of frequent urination and constant thirst) should be referred to the physician as soon as possible in order to be checked. The treatment of diabetes should start before the development of complications. Also, if a patient during dental treatment has symptoms of hyperglycemia (red dry skin, rapid breathing, dehydration, acetone breath), he should be immediately treated.
All patients with extensive periodontal disease which responds poorly to therapy, patients with frequent episodes of candidiasis and patients with severe dryness of the mouth (especially if they complain of frequent urination and constant thirst) should be referred to the physician as soon as possible in order to be checked. The treatment of diabetes should start before the development of complications. Also, if a patient during dental treatment has symptoms of hyperglycemia (red dry skin, rapid breathing, dehydration, acetone breath), he should be immediately treated.
Conclusion
Good control of diabetes minimizes the risk of oral manifestations and to realizes the preconditions for successful dental treatment. Although oral manifestations of diabetes are not life-threatening to the patient, they can significantly reduce their quality of life. In addition, some of them such as gingivitis and periodontitis have adverse effect on disease control. Daily implementation of the oral hygiene measures and regular dental checkups will preserve oral health of patients with diabetes and will contribute significantly to the health of the whole organism.






